|
 |
- Search
|
|
||
Abstract
Objective
Methods
Results
Conclusion
NOTES
ACKNOWLEDGEMENTS
Fig.┬Ā1.

Fig.┬Ā2.
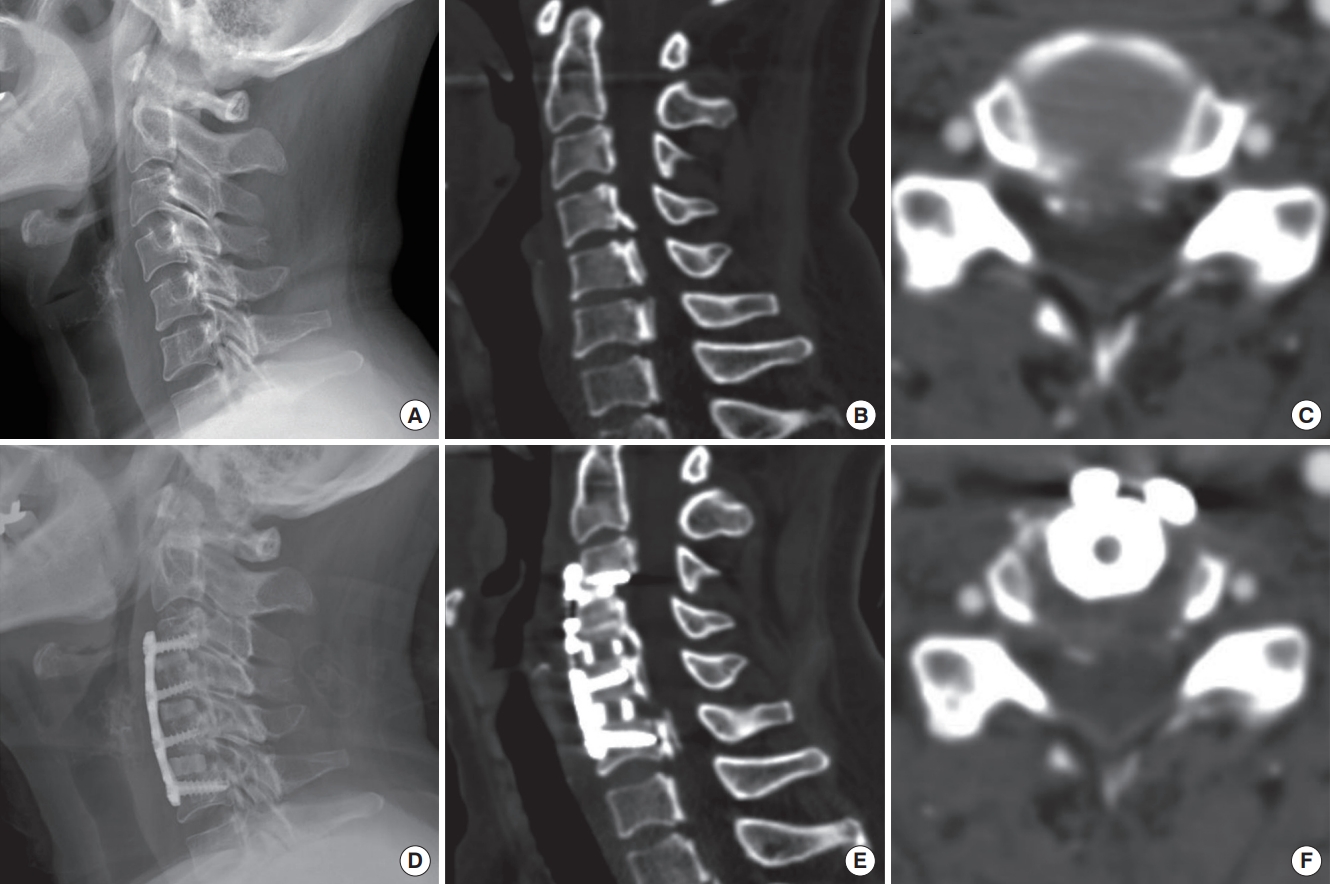
Fig.┬Ā3.

Fig.┬Ā4.

Table┬Ā1.
| Characteristic | VBSO (n = 109) | ACCF (n = 45) | p-value |
|---|---|---|---|
| Male sex | 73 (67.0) | 25 (55.6) | 0.18 |
| Age (yr) | 59.3 ┬▒ 9.8 | 62.1 ┬▒ 9.1 | 0.07 |
| Follow-up period (mo) | 44.8 ┬▒ 23.2 | 82.8 ┬▒ 47.7 | < 0.01* |
| No. of involved levels | 2.8 ┬▒ 0.4 | 2.0 ┬▒ 0.0 | < 0.01* |
| OPLL | 85 (78.0) | 9 (20.0) | < 0.01* |
| DM | 14 (12.8) | 4 (8.9) | 0.49 |
| HTN | 22 (20.2) | 12 (26.7) | 0.38 |
| Malignancy | 2 (1.8) | 0 (0) | 1.00 |
| BMI (kg/m2) | 25.1 ┬▒ 3.2 | 24.5 ┬▒ 3.7 | 0.17 |
| Smoking habit | 16 (14.7) | 5 (11.1) | 0.80 |
| Operation time (min) | 210.2 ┬▒ 37.6 | 203.9 ┬▒ 29.6 | 0.21 |
| Hospital stay (day) | 5.7 ┬▒ 3.4 | 6.2 ┬▒ 3.4 | 0.26 |
Values are presented as number (%) or mean┬▒standard deviation.
VBSO, vertebral body sliding osteotomy; ACCF, anterior cervical corpectomy and fusion; OPLL, ossification of the posterior longitudinal ligament; DM, diabetes mellitus; HTN, hypertension; BMI, body mass index.
Student t-test was used to analyze the age, follow-up period, number of involved levels, BMI, operation time, and hospital stay days; chisquare test or Fisher exact test was used to analyze the number of patients, DM, HTN, malignancy, and current smoker.
Table┬Ā2.
| Variable | VBSO | ACCF | p-value |
|---|---|---|---|
| Perioperative | |||
| ŌĆāNeurologic deterioration | 0 (0) | 2 (4.4) | 0.08 |
| ŌĆāDural tear | 2 (1.8) | 1 (2.2) | 1.00 |
| ŌĆāDysphagia | 8 (7.3) | 6 (13.3) | 0.24 |
| ŌĆāDysphonia | 4 (3.7) | 2 (4.4) | 1.00 |
| ŌĆāC5 palsy | 5 (4.6) | 0 (0) | 0.32 |
| Delayed | |||
| ŌĆāGraft dislodgement | 0 (0) | 2 (4.4) | 0.08 |
| ŌĆāInfection | 0 (0) | 1 (2.2) | 0.29 |
| ŌĆāImplant failure | 3 (2.8) | 4 (8.9) | 0.20 |
| ŌĆāSignificant subsidence | 6 (5.5) | 18 (40) | < 0.01* |
| ŌĆāPseudoarthrosis | 3 (2.8) | 4 (8.9) | 0.20 |
| Others | |||
| ŌĆāReoperation | 2 (1.8) | 5 (11.1) | 0.02* |
Table┬Ā3.
| Variable | VBSO | ACCF | p-value |
|---|---|---|---|
| Neck pain VAS | |||
| ŌĆāPreoperative | 3.1 ┬▒ 2.6 | 3.8 ┬▒ 2.9 | 0.16 |
| ŌĆāFinal | 2.2 ┬▒ 2.2 | 2.4 ┬▒ 2.6 | 0.39 |
| NDI | |||
| ŌĆāPreoperative | 13.9 ┬▒ 8.3 | 17.7 ┬▒ 11.1 | 0.09 |
| ŌĆāFinal | 8.8 ┬▒ 6.8 | 9.6 ┬▒ 6.4 | 0.33 |
| JOA | |||
| ŌĆāPreoperative | 13.4 ┬▒ 2.3 | 14.7 ┬▒ 1.6 | 0.05 |
| ŌĆāFinal | 15.2 ┬▒ 1.9 | 15.9 ┬▒ 1.1 | 0.08 |
| ŌĆāJOA recovery rate | 49.9 ┬▒ 40.8 | 48.4 ┬▒ 43.9 | 0.46 |
| Preoperative alignment | |||
| ŌĆāC2ŌĆō7 lordosis (┬░) | 8.5 ┬▒ 6.7 | 7.5 ┬▒ 8.5 | 0.26 |
| ŌĆāSegmental lordosis (┬░) | 2.2 ┬▒ 12.1 | 0.4 ┬▒ 10.0 | 0.21 |
| ŌĆāC2ŌĆō7 SVA (mm) | 20.2 ┬▒ 12.1 | 19.7 ┬▒ 12.0 | 0.38 |
| Final alignment | |||
| ŌĆāC2ŌĆō7 lordosis (┬░) | 13.9 ┬▒ 7.5 | 10.1 ┬▒ 8.0 | 0.02* |
| ŌĆāSegmental lordosis (┬░) | 15.7 ┬▒ 7.1 | 6.6 ┬▒ 10.2 | < 0.01* |
| ŌĆāC2ŌĆō7 SVA (mm) | 19.9 ┬▒ 9.4 | 18.9 ┬▒ 10.8 | 0.31 |
Values are presented as mean┬▒standard deviation.
VBSO, vertebral body sliding osteotomy; ACCF, anterior cervical corpectomy and fusion; VAS, visual analogue scale; NDI, Neck Disability Index; JOA, Japanese Orthopedic Association; seg, segmental; SVA, sagittal vertical axis.
All variables were analyzed using the Student t-test.
Table┬Ā4.
REFERENCES

- TOOLS